Unveiling the Landscape of the Eye: A Comprehensive Guide to Normal Corneal Topography
Related Articles: Unveiling the Landscape of the Eye: A Comprehensive Guide to Normal Corneal Topography
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Unveiling the Landscape of the Eye: A Comprehensive Guide to Normal Corneal Topography. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Unveiling the Landscape of the Eye: A Comprehensive Guide to Normal Corneal Topography
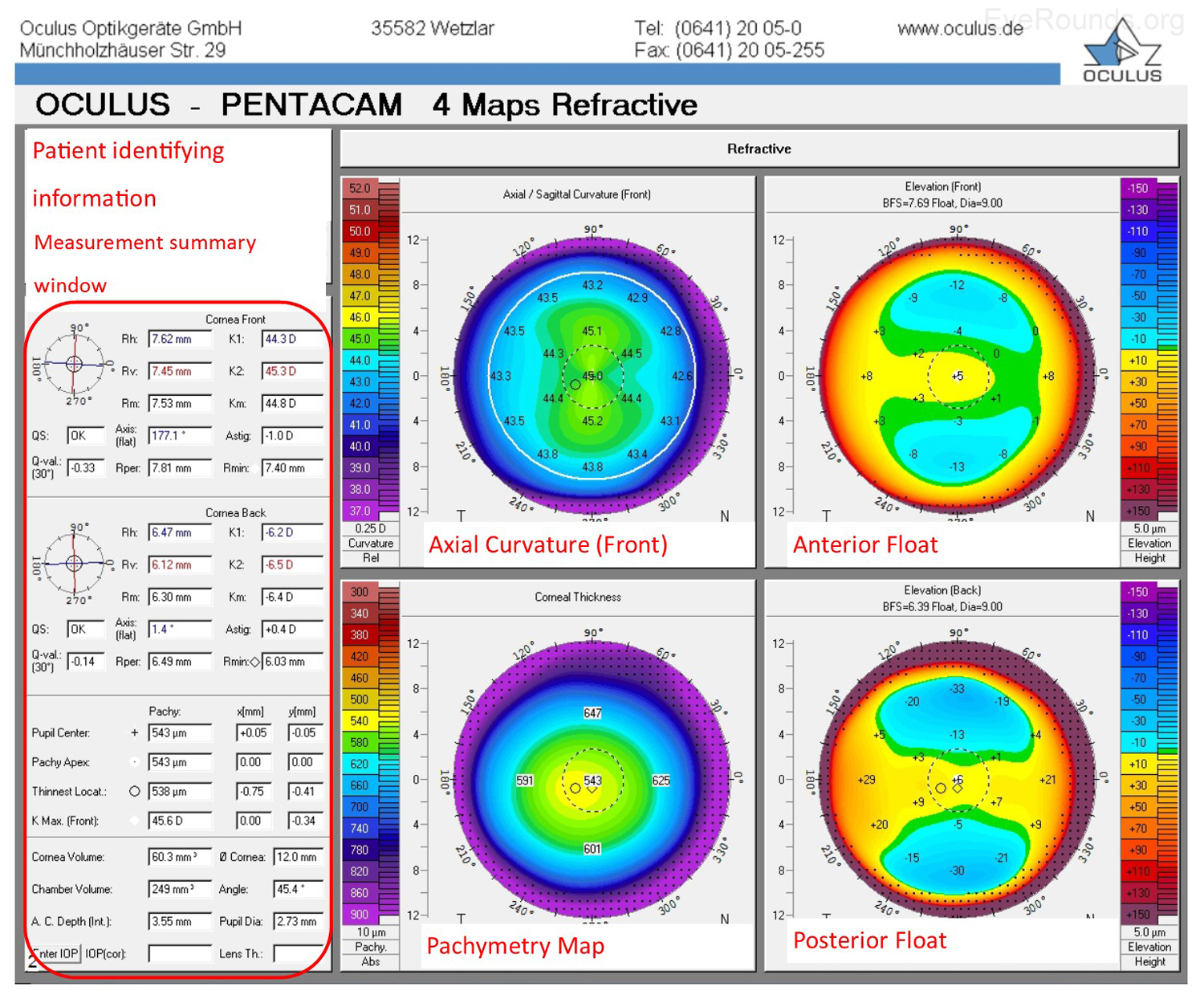
The cornea, the transparent outer layer of the eye, plays a crucial role in focusing light onto the retina, enabling clear vision. Its intricate shape, with a gentle curve, is paramount to this function. Corneal topography, a non-invasive imaging technique, maps this curvature, providing a detailed representation of the cornea’s surface. This map serves as a valuable tool for understanding corneal health, diagnosing conditions, and guiding treatment decisions.
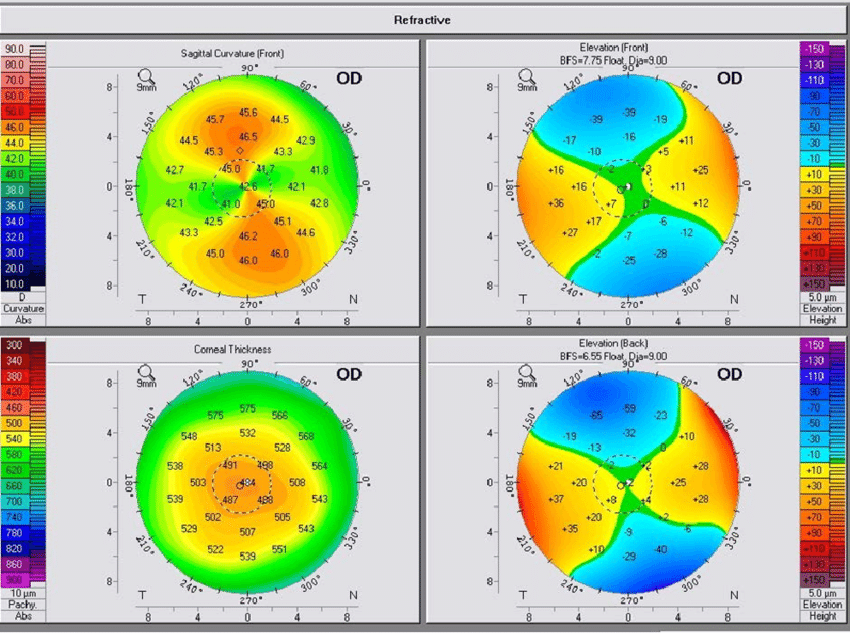
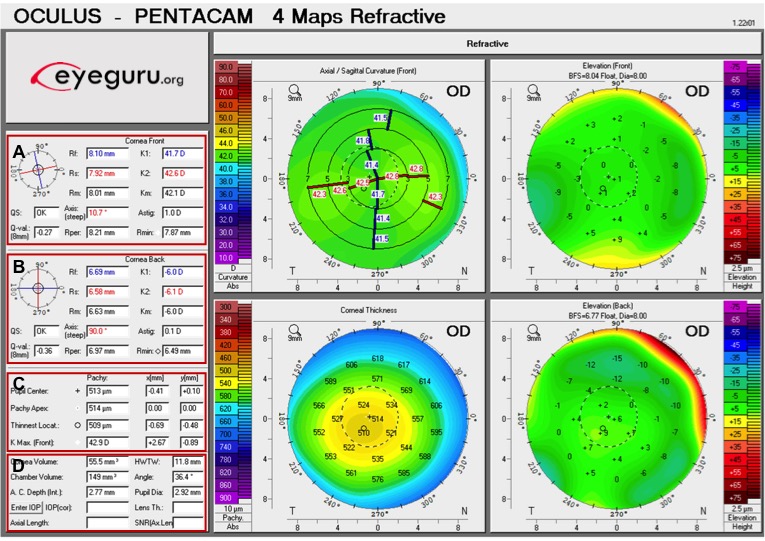
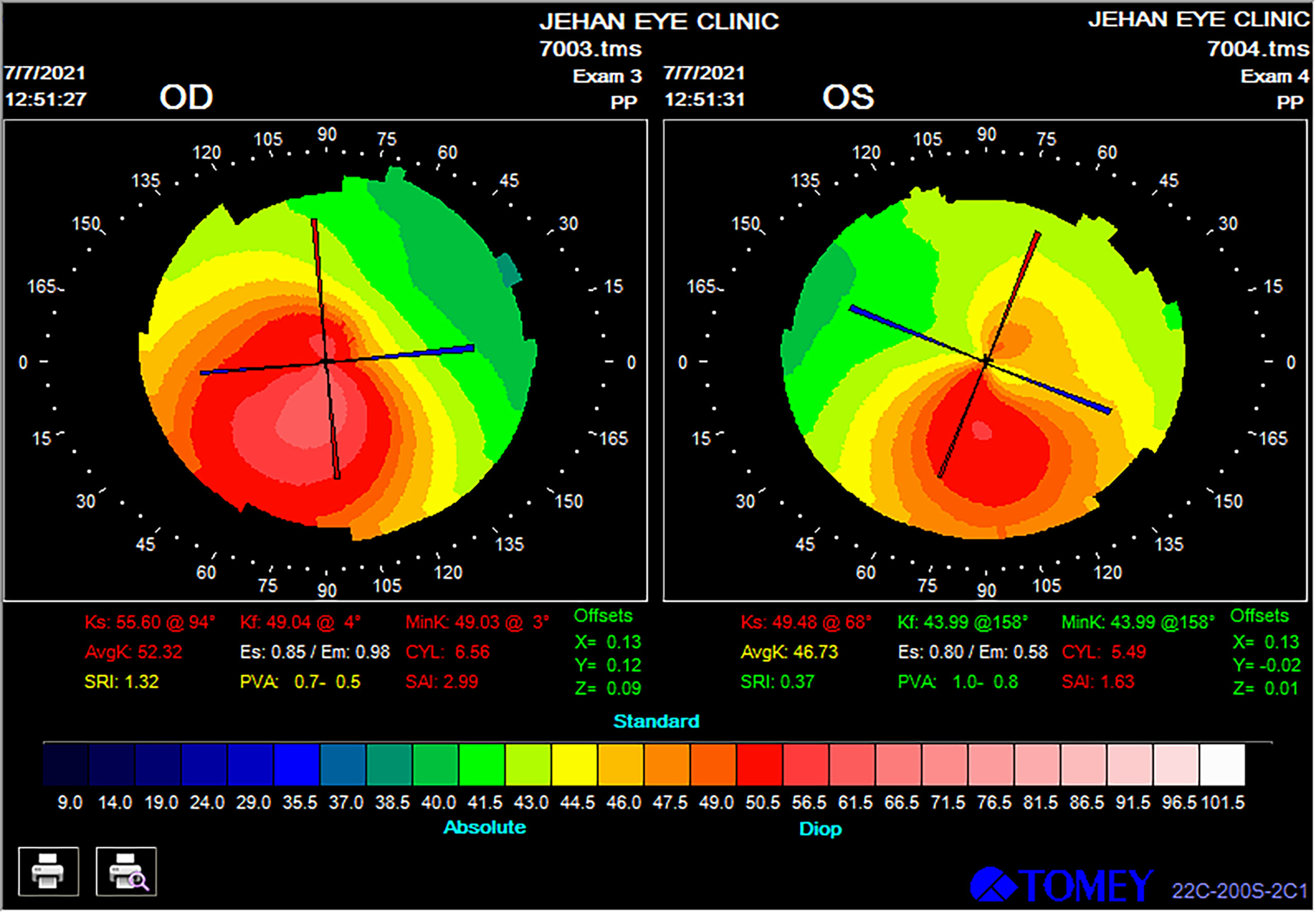
Understanding the Map: A Visual Representation of Corneal Shape
A normal corneal topography map resembles a contour map, with lines representing elevations and depressions on the cornea’s surface. Each line, known as an "isopter," connects points of equal elevation. The center of the cornea, the apex, is typically the highest point, indicated by the innermost isopter. As the lines extend outwards, they represent progressively lower elevations, depicting the gradual flattening of the cornea towards its periphery.
Key Features of a Normal Corneal Topography Map
A normal corneal topography map exhibits distinct features that reflect a healthy cornea:
- Symmetry: The map displays a symmetrical pattern, with the right and left sides mirroring each other. This symmetry indicates consistent curvature across the corneal surface.
- Regularity: The isopters are smooth, continuous, and evenly spaced, demonstrating a regular and consistent corneal shape.
- Central Apex: The map clearly identifies a central apex, signifying the highest point on the cornea. This apex is essential for optimal light focusing.
- Gradual Flattening: As the isopters extend outward from the apex, they gradually flatten, indicating a smooth transition from the central curvature to the peripheral cornea.
- Absence of Irregularities: The map should be free from any abrupt changes, peaks, or valleys, signifying a smooth and uniform corneal surface.
Interpreting the Map: Unveiling Potential Corneal Abnormalities
Deviations from these normal features can signal underlying corneal conditions:
- Asymmetry: Uneven distribution of isopters, with one side differing significantly from the other, could indicate corneal asymmetry, potentially caused by conditions like keratoconus or irregular astigmatism.
- Irregularity: Discontinuous or unevenly spaced isopters suggest corneal irregularities, potentially indicative of scarring, ectasia, or other corneal deformities.
- Central Depression: A central depression, characterized by the apex being lower than the surrounding corneal surface, may signal keratoconus, a progressive corneal thinning disorder.
- Steepening or Flattening: Abnormal steepening or flattening of the corneal curvature can affect refractive error, leading to blurred vision.
The Significance of Corneal Topography: A Powerful Diagnostic Tool
Corneal topography plays a vital role in ophthalmic practice, offering numerous benefits:
- Early Detection: It allows for early detection of corneal conditions like keratoconus, which can progress silently, leading to significant vision impairment if left untreated.
- Accurate Diagnosis: Corneal topography provides a detailed visual representation of the cornea, aiding in the accurate diagnosis of various corneal conditions, including refractive errors, corneal ectasia, and corneal dystrophies.
- Personalized Treatment Planning: The map guides the selection of appropriate treatment options for refractive surgery, contact lens fitting, and other corneal procedures.
- Monitoring Disease Progression: Corneal topography enables the monitoring of corneal disease progression over time, allowing for timely interventions and adjustments to treatment plans.
- Pre-operative Assessment: It helps assess corneal suitability for refractive surgery, ensuring optimal outcomes and minimizing potential complications.
FAQs: Addressing Common Questions
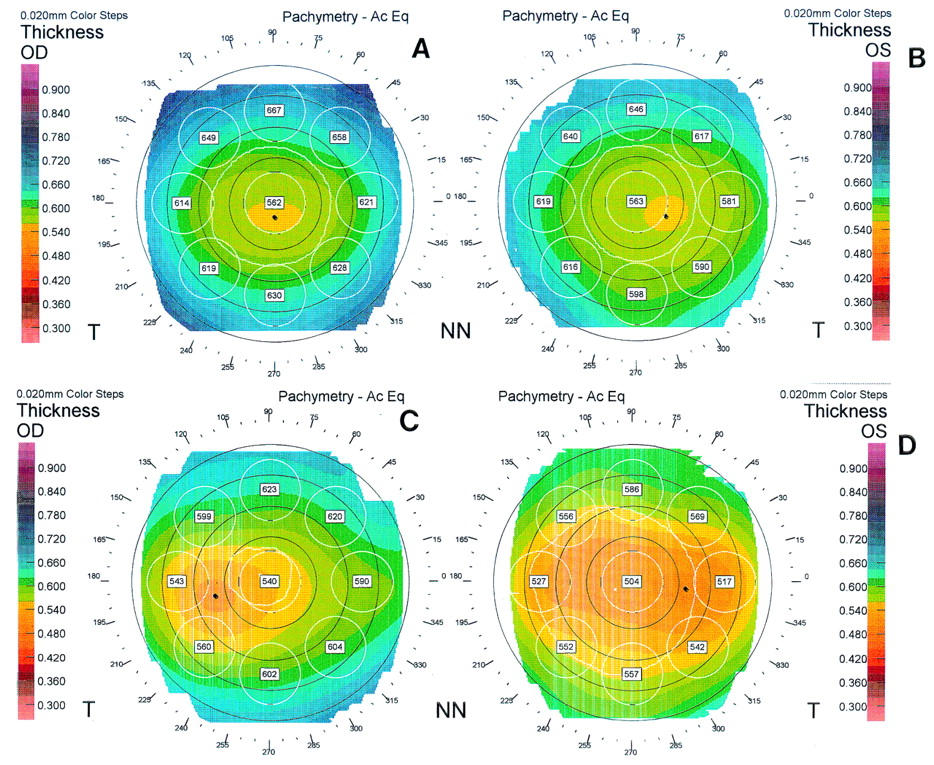
Q1: What is the difference between corneal topography and corneal pachymetry?
A: While both techniques assess corneal characteristics, they focus on different aspects. Corneal topography maps the corneal surface curvature, providing a detailed representation of its shape. Corneal pachymetry measures corneal thickness, providing information about its overall thickness and potential thinning areas.
Q2: How often should I get a corneal topography test?
A: The frequency of corneal topography tests depends on individual factors, such as age, family history of corneal conditions, and existing eye conditions. Regular tests are recommended for individuals with a history of corneal issues, those undergoing refractive surgery, and those with risk factors for corneal diseases.
Q3: Is corneal topography a painful procedure?
A: Corneal topography is a painless and non-invasive procedure. It involves scanning the cornea with a light beam, similar to taking a picture.
Q4: What are the limitations of corneal topography?
A: While corneal topography is a valuable tool, it has some limitations:
- Operator Dependence: The accuracy of the map can be influenced by the operator’s skill and experience.
- Eye Movement: Eye movements during the test can affect the map’s accuracy.
- Limited Depth Information: Corneal topography primarily focuses on the surface curvature, providing limited information about corneal thickness or internal structures.
Tips for Enhancing the Accuracy of Corneal Topography
- Maintain Eye Stability: Minimize blinking and eye movement during the test.
- Clear Contact Lenses: Remove contact lenses before the test, as they can distort the map.
- Follow Instructions: Adhere to the operator’s instructions for proper positioning and eye fixation.
- Regular Tests: Undergo regular corneal topography tests, especially if you have a history of corneal conditions or are undergoing refractive surgery.
Conclusion: The Importance of Understanding the Corneal Landscape
Corneal topography provides a window into the intricate landscape of the cornea, revealing its unique curvature and potential abnormalities. This valuable tool empowers ophthalmologists to diagnose and manage corneal conditions effectively, ensuring optimal eye health and vision. By understanding the nuances of corneal topography, patients can actively participate in their eye care journey, making informed decisions about their vision and overall health.




Closure
Thus, we hope this article has provided valuable insights into Unveiling the Landscape of the Eye: A Comprehensive Guide to Normal Corneal Topography. We hope you find this article informative and beneficial. See you in our next article!